The needs and goals of a person who is facing a serious or terminal illness are different from the needs of most other clients. For many, the main goal will focus on relaxation and comfort versus any expectation around complete symptom relief or recovery.
In the past, many people associated palliative and hospice care with helping people manage the process of dying. Today, however, the goal is understood to be much more broad and include, among other things, maintaining or improving quality of life and managing troublesome symptoms.
Palliative care especially is aimed at helping people with chronic, life-limiting or serious illnesses manage symptoms, as well as the side effects of treatment. This care can span the course of the illness, and is provided alongside other ongoing medical treatment and integrative care strategies.
Importantly, as is often seen in integrative health care approaches, palliative care is a team effort and can include doctors, nurses, social workers, spiritual services and, yes, massage therapists.
The Basics of Palliative Care
Using massage therapy as part of an overall health care strategy for clients receiving palliative care is an approach, not a specific type of massage technique. Massage sessions used for palliative care are comfort-focused, often shorter than traditional massage sessions, and may aim to help clients better manage symptoms like pain, nausea, anxiety and depression, and sleep issues.
“Compared to traditional massage therapy, palliative care seeks to help clients just feel better, and not effect a particular therapeutic change or outcome, such as reducing muscle tension, loosening adhesions or even integration,” says Michael Patrick, LMT, owner at Centered Presence. “It is simply to calm, soothe and comfort.”
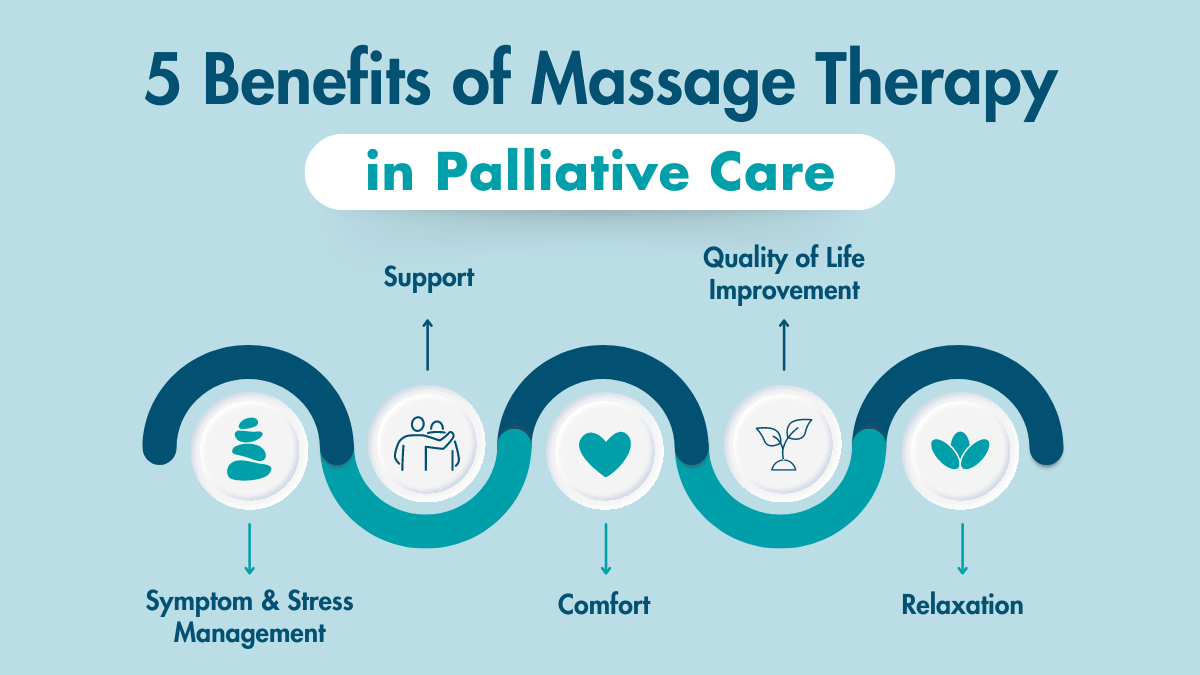
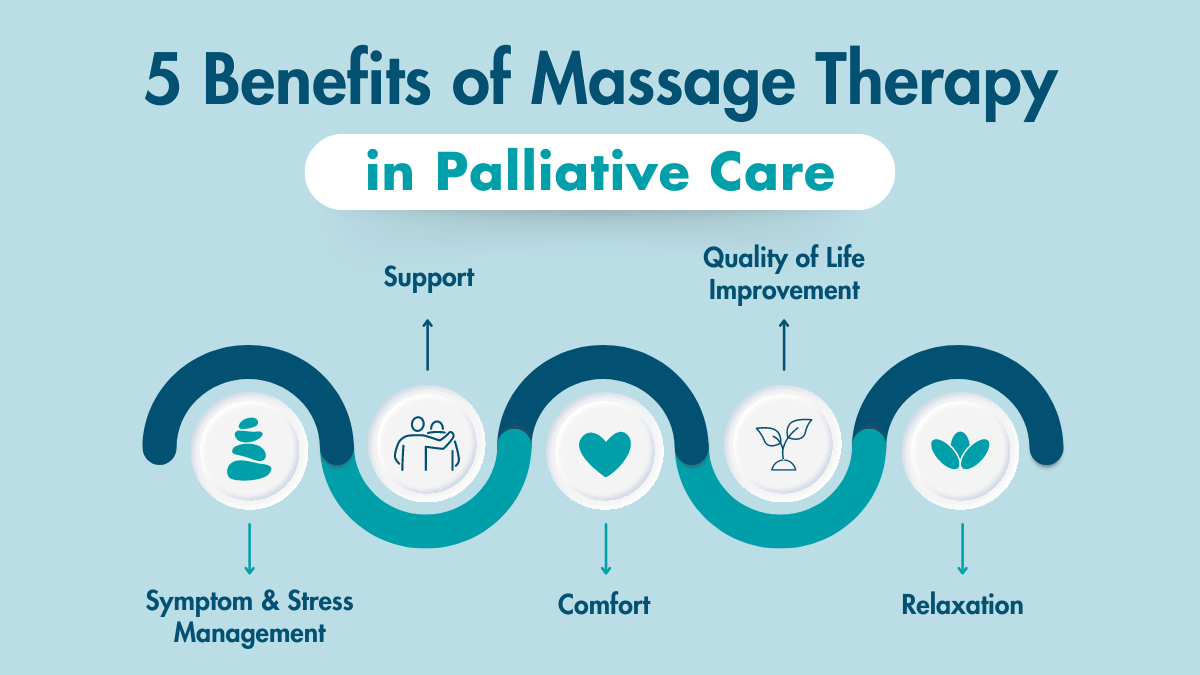
Symptom relief is also a benefit of palliative care, and massage therapy has shown real benefit, according to Joseph David Elder, MA, LMT. “Massage therapy for palliative care patients is used for symptom and stress management, comfort, quality of life improvement, support, and relaxation, and not rehabilitation,” he explains.
Related: Research on Benefits of Massage in Palliative Care
“Palliative massage aims to invoke the parasympathetic nervous system,” Patrick adds. “It does this in a very gentle, accessible pace that allows clients to receive benefits without inadvertently creating resistance.”
Additionally, the guidance often provided by a massage therapist during a session, such as meditation cues or therapeutic positioning instructions, can help to improve a client’s self-care skills, quality of life and comfort between massage sessions.
Massage Benefits and Contraindications When Working With Palliative Care Clients
Recent research continues to build on what is currently understood about the role massage therapy plays in integrative health care approaches like palliative care, reinforcing the benefits some massage therapists are seeing with these clients.
A 2022 study1 exploring the feasibility and acceptability of caregiver massage therapy for patients in palliative care, patients’ and caregivers’ experience of massage therapy, and the staff perspectives about caregiver massage therapy in palliative care, followed patients who were offered massage therapy from a caregiver who had been trained in a massage protocol.
Caregiver massage therapy was provided up to five days post training, and both patients and caregivers completed self-report measures of satisfaction. Additionally, caregivers rated massage-related burden and confidence.
Researchers noted that both caregivers and patients were satisfied with the massage training sessions, and patients reported perceptions of comfort during subsequent sessions.
The study concluded that caregiver massage training is feasible, with patient symptom improvement and caregiver empowerment cited as benefits. However, caregivers did make note that massage could potentially become burdensome for them.
A 2023 three-armed randomized trial2 compared three different doses of therapist-applied massage among adult hospitalized patients receiving palliative care consultation to better understand optimal dosage of massage. Dosing including a 10-minute daily massage for three days, a 20-minute daily massage for three days and a single 20-minute massage.
Researchers were looking for changes in overall quality of life and symptom management. The primary outcome measure was the single-item McGill QoL question. Secondary outcomes measured included pain/symptoms, rating of peacefulness and satisfaction with the intervention.
Results suggest that all three dosing groups demonstrated within-group quality of life improvement at follow up. No significant between-group differences were found.
“Massage therapy in complex patients with advanced illness was beneficial beyond dosage,” researchers noted. “Findings support that session length (10 or 20 minutes) was predictive of short-term improvements while treatment frequency (once or three consecutive days) predicted sustained improvement follow-up.”
Massage dosing was also investigated in a 2023 seven-arm randomized trial in palliative cancer care.3 Dosing comprised weekly massage for four weeks as prescribed (15-, 30- or 60-minutes; 2x or 3x per week) and a four-week follow-up.
Pain and fatigue intensity, as well as sleep disturbances, were measured using a 0 to 10 scale at baseline, weekly during the intervention and at the follow-up.
Results suggest the odds of clinical improvement significantly increased with dose escalation, and the effects durability was significantly shorter at 15-minute doses compared to 30- and 60-minute doses.
Although symptom improvement did not significantly differ between 2x per week versus 3x per week massage, the effect durability for 3x per week dosing was significantly higher.
“The findings indicated that dose-escalation increases the efficacy of massage for pain-fatigue-sleep syndrome cluster,” researchers noted. “Although the 60-minute doses were found to be more effective, the 30-minute doses can be considered more practical because they are less costly and time-consuming.”
The usual contraindications for massage, such as fever and contagious disease, still apply when working with palliative care clients.
Because massage during these session is typically much lighter, slower and often only applied to the extremities, however, contraindications most often depend on the comfort of the client. Good reminders are to be aware of and avoid any medical devices or tubing, or open wounds.
Intake and Massage Sessions: What Massage Therapists Need to Know
Information You Need
Intake is always important, but especially so when working with clients who are seeking massage for palliative care. Massage therapists need a good understanding of the client’s medical history and current health status to best tailor a massage session to client comfort.
Some information on how a client is dealing with their condition can also help, though massage therapists need to ensure they’re clear about their ethical boundaries.
“I still need to know about their medical conditions in a traditional intake, but the emotional component of how they relate to their condition or how it has affected them emotionally is particularly relevant,” Patrick says.
“Remember, the aim isn’t to fix anything in the therapeutic sense, but, at least for the time of the session, to shut down the stress response so that the body’s natural processes can get some airtime,” he adds.
Massage Session Basics
The very nature of this work means that massage sessions can vary greatly in length, anywhere from 15 to 90 minutes, depending on how the client is feeling.
Typically, shorter sessions (20 to 30 minutes) are preferred, and decisions around positioning and massage techniques used should be decided upon based on both a client’s preferences and a massage therapist’s best judgment.
“The massage table may be impossible for the client to lay on due to their illness, muscle soreness or disability,” says Erica Johansen, LMT. “Being flexible is key. Bolsters and pillows may be used to help prop the client into a comfortable position.”
Additionally, massage therapists working with palliative care clients need to be adaptable and willing to meet the client where they are, both in session and location, as many times massage will take place in a person’s home or medical facility, whether hospital, rehabilitation center or assisted living environment.
A typical session will include some type of guided mind and body relaxation practices, gentle touch (such as reflexology or acupressure) for parts of the body, such as the hands or feet, and comfort-focused effleurage and/or manual lymphatic drainage.
Massage sessions can be done with or without lotion, and many clients will remain clothed. When it comes to technique, the key is to be slow and gentle.
“Slow, slow, slow,” says Patrick. “If you think you are going too slowly, you probably could still go slower. Think of it as a snail’s pace, and just as much pressure.”
When working with clients outside your massage practice, remember to return the client’s bedrail heights, bed heights, meal trays—anything you might have moved during the session—back to the position they were found in once a massage has ended.
Self-Care: How Massage Therapists Can Care for Themselves
One thing for massage therapists to consider about this slow pace is that it can actually feel more strenuous on their own bodies than giving a regular massage or even a heavy-pressure massage.
This is due to the sustained muscle control necessary to perform the very slow, controlled movements. The oftentimes awkward accessibility sometimes found in these client’s homes or hospital rooms can also add to the strenuous nature of the work.
“Massage feels so good for palliative care patients,” says Patrick. “However, it draws on my resources as a therapist differently than Swedish massage does. If I don’t replenish those resources, I have nothing to give.”
It isn’t just the physical side of things that can be draining on a massage therapist. It can be an emotionally difficult experience, too.
“This is deeply rewarding and challenging work that isn’t for the faint of heart or the weak of stomach,” says Elder. “It requires ongoing learning, and a genuine desire to be of service to those who are suffering and in difficult situations.”
A nationwide survey4 of physicians, physician assistants and nurse practitioners in palliative care documented recommendation rates of integrative care therapies for target symptoms of palliative care patients.
The survey found that massage was the third most recommended integrative care modality behind mind-body interventions like meditation and biofeedback. Pain, anxiety, mood disturbance and distress were the most targeted symptoms.
Overall, palliative massage is one component of an integrative care plan that can bring comfort and symptom relief to clients in need. “Interdisciplinary interventions such as massage therapy help manage symptoms while improving a patient’s well-being and quality of life experience,” Elder says.
Palliative Care vs Hospice Care: What is the Difference?
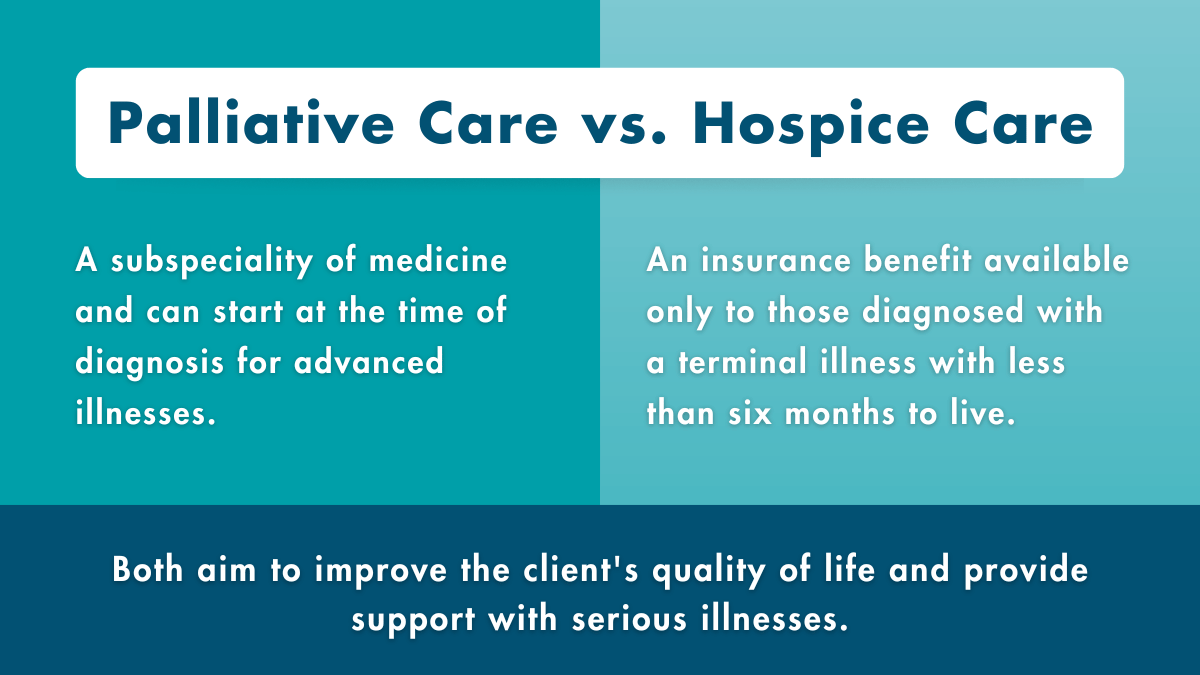
Palliative care and hospice care have many similarities. Both are concerned with improving or maintaining a person’s quality of life. Both, too, center a client’s needs and are meant to help a patient deal with serious illness.
Related: Massage & Hospice
There are, however, a few key differences, one being when care can begin. “The main difference between palliative care and hospice is that palliative care is a subspecialty of medicine and can start at the time of diagnosis for advanced illnesses, whereas hospice is an insurance benefit available only to those diagnosed with a terminal illness and have less than six months to live,” Tara Liberman, DO, executive director of Northwell Health’s Hospice Care Network said in an article for Northwell Health’s Insights.
“But," she continues, "whether you’re seeing a palliative care or a hospice specialist, the goal is always to identify the cause of someone’s discomfort, then find different ways to relieve that pain.”
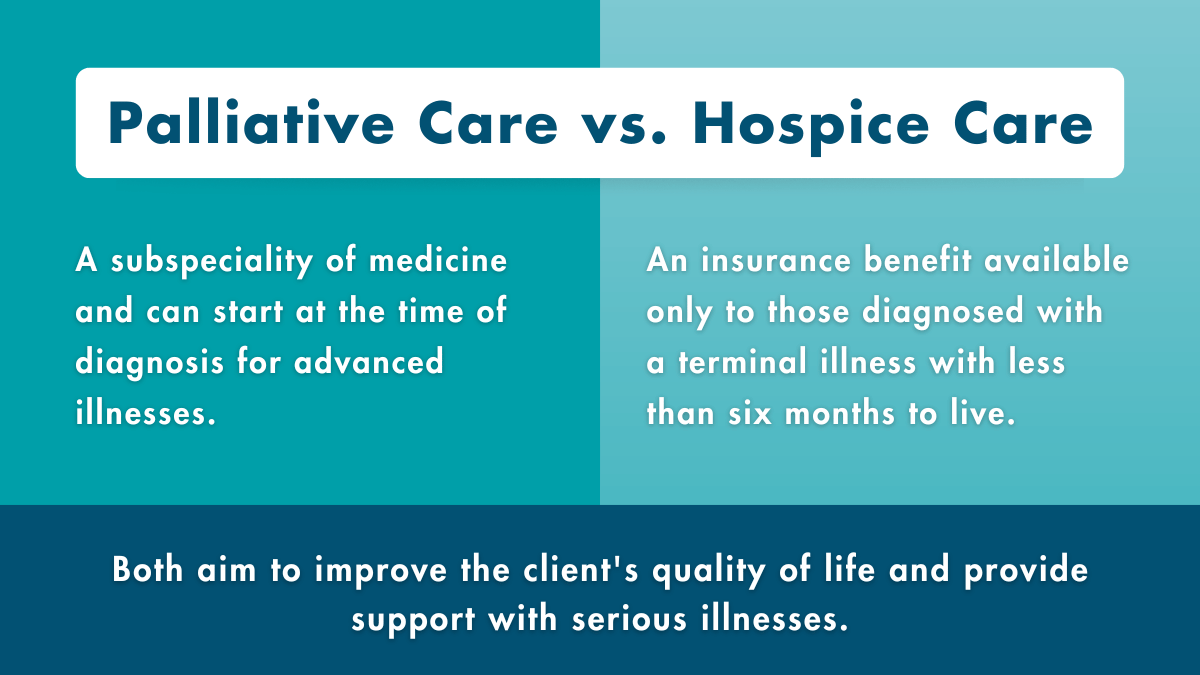
For massage therapists specifically, however, massage for both of these populations remain largely unchanged. “There is a difference between palliative care and hospice care,” says Erica Johansen, LMT. “Though the massage is much the same in terms of it being a lighter massage, not a deep tissue massage. Sometimes clients receiving palliative care transition to hospice care.”