Massage Therapy Journal
In Safe Hands: Massage & PTSD
Clients with PTSD may find relief from stress, anxiety and depression with massage therapy.
Massage therapy has shown promise in helping to alleviate some of the symptoms associated with PTSD.
By David Malone, August 1, 2024
Post-traumatic stress disorder (PTSD) is a common term that is too often misunderstood. While it’s true that PTSD may develop after a traumatic event, not all traumatic events necessarily lead to PTSD.
The U.S. Department of Veterans Affairs (VA) defines PTSD this way: “The word ‘trauma’ is used for many different types of experiences that are stressful. But not all stressful events are the type of trauma that can lead to PTSD. To be at risk for PTSD, the trauma must be a shocking and dangerous event that you see or that happens to you. During this type of event, you think that your life or others’ lives are in danger.”
About six of every 100 people in the U.S. will have PTSD at some point in their lives, according to va.gov. In 2020, an estimated 13 million Americans had PTSD.
Additionally, veterans are more likely to have PTSD than civilians, and veterans who have been deployed to a war zone are more likely than those who did not deploy. Seven out of every 100 veterans will develop PTSD, according to the VA.
The National Institute of Mental Health describes the following guidelines for diagnosing PTSD, suggesting that all of the following symptoms must be present for at least one month:
Massage therapy has been shown to help with some of these symptoms.
“My experience with massage therapy as it relates to PTSD is that it aids down-regulation of the sympathetic nervous system,” says Matthew Howe, HB, LMT, ICST, founder, instructor and therapist, Touch Education. “This can produce positive benefits that address hyper-vigilance, exaggerated startle response, problems in concentration and sleep disturbances.”
Interest in integrative health care approaches continues to grow, especially among veterans, as partly evidenced by the VA’s recent expansion of health care offerings. As data start to be collected, early results indicate integrative therapies like massage therapy may have a very real role to play in veteran health care.
A 2023 study1 explored the questions of how many VA patients would use integrative approaches and chiropractic care if they were available at modest to no fee, and if patients with some health conditions or characteristics would be more likely than others to use these therapies.
Researchers used electronic medical records to conduct a three-year, retrospective analysis of VA patients’ use of 11 VA-covered therapies, including but not limited to massage therapy, chiropractic care and acupuncture.
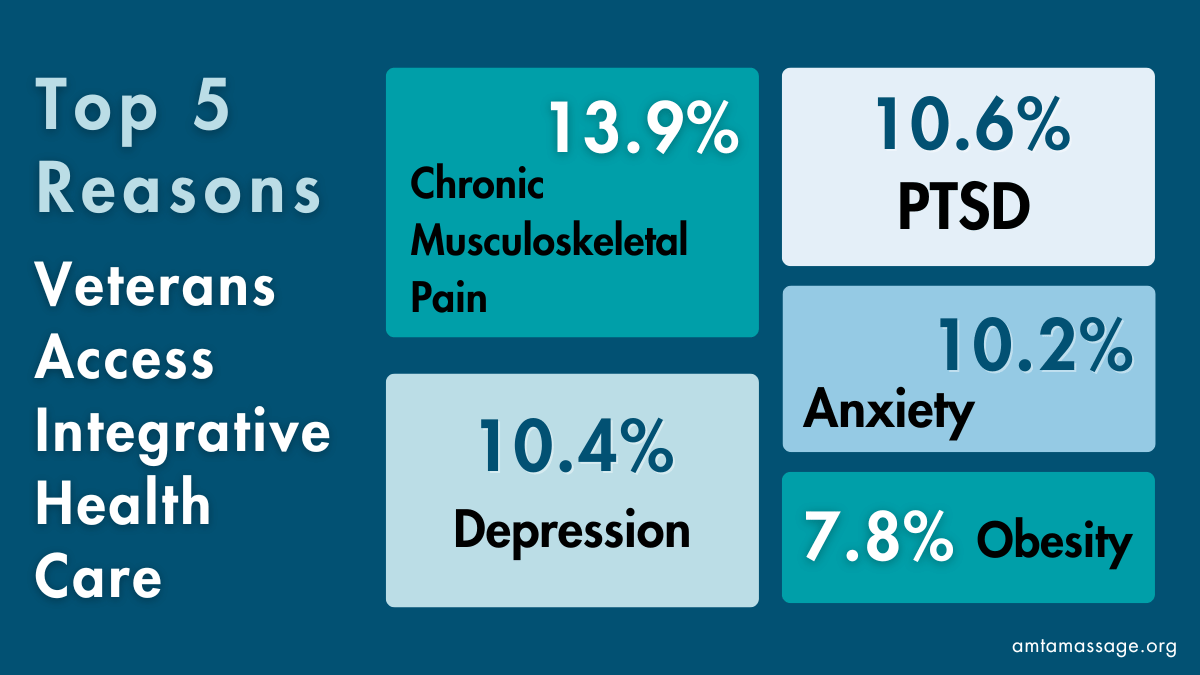
The analysis found that veterans’ use of integrative approaches increased by 70% in three years (October 2016 to September 2019), with use among all VA patients reaching 5.7% by 2019. The top five most common reasons veterans accessed integrative health care included:
Additionally, women were more likely than men to seek these approaches.
Researchers noted that the veterans’ rapid adoption of integrative health care approaches could help shape federal and state health policy to guide other health care institutions that are considering providing this care.
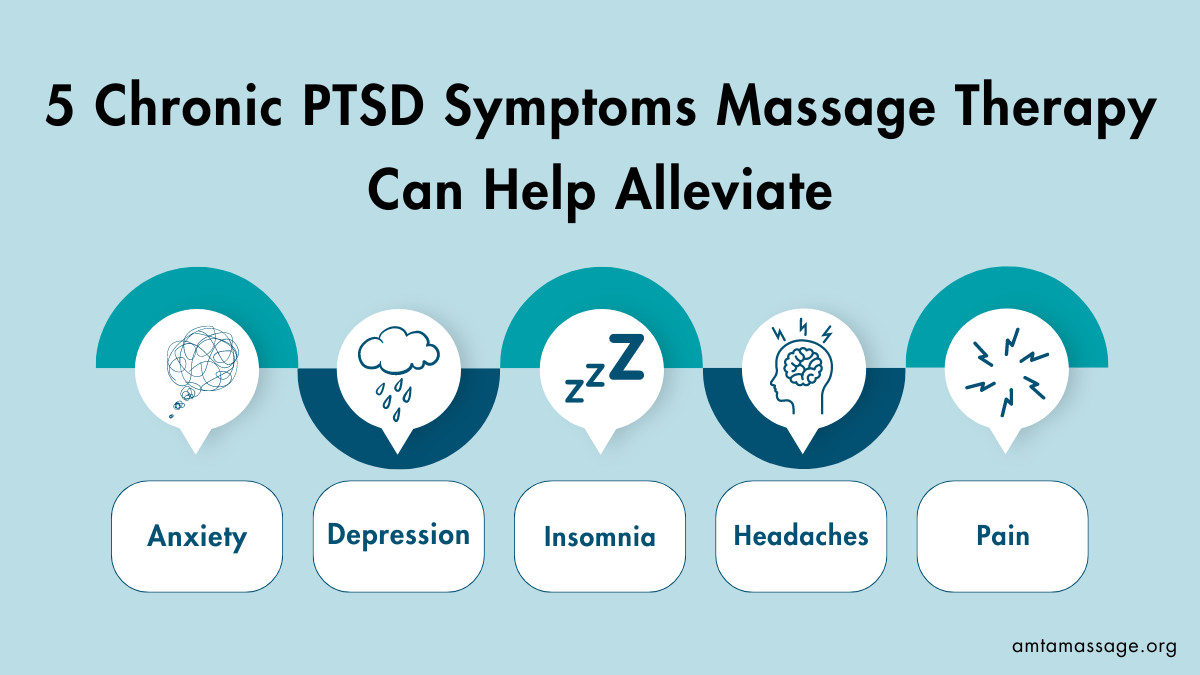
Before considering the benefits massage therapy may have for people with PTSD, understanding some of the effects of trauma—such as an internalized lack of safety, a high degree of anxiety or depression, difficulty sleeping, and challenges with social relationships—is important.
“If you look at the literature, it becomes apparent that massage therapy can help with anxiety, depression and/or insomnia. These benefits have been documented many times,” says Pamela Fitch, M. Ad. Ed., RMT. “However, with a traumatized population, such massage therapy benefits come with significant therapist responsibilities. It is not possible to help someone with anxiety unless they feel safe. That becomes the first order of inquiry and the most essential part of the treatment.”
A pilot study2 examined the effects of light touch manual therapies (LTMT) on headache, anxiety and other symptoms experienced by active duty United States service members with chronic PTSD. Ten service members who were diagnosed with PTSD and suffered a self-reported head injury were provided two hour-long sessions of mixed LTMT given one week apart. Data to assess the effects were gathered before and after each session.
The results showed that headache, anxiety and pain interference were significantly reduced during the course of the pilot study, suggesting that LTMT may be helpful in reducing some of the symptoms of PTSD and head injury.
For massage therapy to be as effective as possible, however, the right type of massage technique needs to be used at the right time. “Any tradesperson will tell you, ‘The right tool for the right job makes any job simpler,’” says Howe. “We use rocking to identify and assess areas of the body that are resistant to movement. It is a simple, non-invasive technique that allows the therapist to locate regions contributing to the client’s current state.”
This type of therapeutically applied rocking can help the client recognize and potentially release holding patterns, Howe adds, while also reducing the sensitivity to external triggers.
“The actual hands-on work is basic and not complicated because clients may not even be able to tolerate touch or deep work,” Fitch says. “My role is to ensure that the client is comfortable with whatever I do and wherever I suggest that we work. That is the most important piece of the therapeutic alliance.”
Craniosacral therapy might also be a good choice, especially for clients who may need help interacting with their resistance or restriction. Here, massage therapists can help to facilitate the release of tension areas that cause operational drag.
Additionally, the light touch of craniosacral may allow the client’s nervous system to shift from a stress response (sympathetic) to a recovery response (parasympathetic), which can be especially important for clients with PTSD. “Often, an individual living with PTSD struggles to calm down or down-regulate,” explains Howe. “They may be touch averse. They get stuck in a sympathetic nervous response, also known as fight/flight.”
“Massage therapy can be easily integrated with other approaches,” says Howe. “Collaboration of care with other health care providers can be a valuable asset.”
Fitch agrees, and also offers a reminder about scope of practice. “Massage therapists should consider integrating their services with other health care professionals who have trauma-informed training,” she says. “Massage therapists do not have the training to navigate these therapeutic relationships as talk therapists and should never try to do both massage therapy and talk therapy.”
An older 2005 study3 explored the commingling of integrative therapies—including massage, acupuncture and Reiki—into community mental health practice. The pilot study was conducted using interview data before and self-report instruments after participants completed a brief program of integrative therapy accompanying ongoing psychotherapy.
The 25 participants, all of whom had experienced trauma and were receiving ongoing psychotherapy, were assigned to a single modality of integrative therapy based on clinical judgment, availability of practitioners and client interest. After receiving the assigned therapy, participants completed an investigator-generated instrument with Likert-scaled ratings of satisfaction and perceived changes in four dimensions of trauma recovery.
The study found all participants reported high levels of satisfaction and significant levels of perceived change on each outcome measure, suggesting that using integrative therapies in community mental health practice may hold promise of enhancing mental health outcomes and improving quality of life.
Working as part of a larger integrative health care team does require massage therapists communicate well with both the client and other health care professionals, while also remaining HIPAA compliant. “I’ll ask how other therapies are going, what their goals are, and what progress they’re making,” Howe says. “I am always open to professional relationships that support clients’ growth.”
In some instances, individuals who have been diagnosed with PTSD may not always disclose their diagnosis to their massage therapist. With PTSD—or any type of mental health condition—there is often still a stigma attached, even as we’re getting better about talking about mental health more generally.
Clinicians in complementary medicine fields, such as massage therapy, will likely treat many with PTSD without knowing it.
A retrospective case report4 exploring the benefits of massage for combat injuries in a veteran with undisclosed PTSD explains: “Mental illness also carries the weight of stigma, which increases a likelihood of nondisclosure whether care is sought or not … Specifically, veterans may seek clinical care from providers who are not privy to medical records and/or provide complementary or alternative care approaches. Because such clinicians rely solely on care recipients to self-report PTSD and those with PTSD have low disclosure rates, clinicians in complementary medicine fields, such as massage therapy, will likely treat many with PTSD without knowing it.”
The case report reviewed a therapeutic encounter between a massage practitioner and a veteran seeking massage therapy for a combat injury. The veteran did not disclose their PTSD diagnosis until two years after initially receiving massage.
Disclosure of PTSD was made during follow-up communication around missed massage appointments, where researchers noted the participant stated the following when asked about the reason for nondisclosure: “It isn’t something you just tell people. For the most part, you just live with it. Most people don’t understand.”
“Working with trauma survivors can be complex and challenging, but it can also be simple. We aim to help humans human better through healthy touch in a safe, supportive environment where they are empowered to take their next steps in healing.”
Matthew Howe
According to researchers, the client’s stated goals of increased range of motion, reduced chronic pain of the injured limb and increased activity in previously enjoyed physical activities were achieved with massage. Additionally, insights around PTSD and clients who might not disclose a mental health condition were also discussed.
“Awareness of these issues is particularly needed among those who work with veterans because core symptoms of PTSD can exacerbate typical responses, increase nondisclosure likelihood, and create barriers to treatment commitment or response less recognized in civilian care settings,” researchers noted. “Inconsistent foundation massage education in the United States limits the systematic inclusion of such essential topics in clinicians’ early training, potentially leaving massage professionals ill-prepared to meet the growing needs of consumers regarding trauma and/or PTSD.”
A word of caution, however. Although understanding, awareness and education around the symptoms and behaviors associated with trauma are key to success, massage therapists should not attempt to pry information out of clients, especially veterans who might be particularly uncomfortable talking about their experiences. “We do not need the client to tell their story to help them,” says Howe. “They are welcome to share, but discussing details of their trauma may not bring benefit to our treatment process.”
Howe says that when working with clients with PTSD, for both those who have disclosed a diagnosis and those who haven’t, intense emotional responses can happen. When they do happen, Howe suggests staying present with the client as they process what they are feeling. “Our hands remain engaged,” he explains. “As long as the client is comfortable, we let them know we are right there with them and they are safe at that moment.”
Regardless if a veteran (or any other client) has PTSD, whether they disclose it or not, massage can provide both physical and emotional benefits. Yes, knowing about a client’s PTSD may help to better plan and guide a massage session, but the environment should be one of safety and comfort in all cases.
“Working with trauma survivors can be complex and challenging, but it can also be simple,” says Howe. “We aim to help humans human better through healthy touch in a safe, supportive environment where they are empowered to take their next steps in healing.”
1. Taylor SL, Gelman HM, DeFaccio R, Douglas J, Hawrilenko MJ, McGinty NK, Resnick A, Tomlanovich NC,Toyama J, Whitehead AM, Kligler B, Zeliadt SB. “We Built it, But Did They Come: Veterans’ Use of VA Healthcare System-Provided Complementary and Integrative Health Approaches.” J Gen Intern Med. 2023 Mar;38(4):905-912.
2. Davis L, Hanson B, Gilliam S. “Pilot study of the effects of mixed light touch manual therapies on activeduty soldiers with chronic post-traumatic stress disorder and injury to the head.” J Bodyw Mov Ther. 2016 Jan:42-50.
3. Collinge W, Wentworth R, Sabo S. “Integrating complementary therapies into community mental health practice: an exploration.” J Altern Complement Med. 2005 Jun;11(3):569-74.
4. Rosenow M, Munk N. “Massage for Combat Injuries in Veteran with Undisclosed PTSD: a Retrospective Case Report.” Int J Ther Massage Bodywork. 2021 Mar 1:4-11.