Nerve pathologies are a common soft-tissue complaint that many massage therapists encounter in practice. Yet, a comprehensive understanding of the nervous system is often not a part of entry-level training for many massage therapists.
The Basics: Pathologies at the Nerve Root vs. Distal from the Nerve Root
A pathological condition at the nerve root level is referred to as a radiculopathy. Symptoms from a radiculopathy are often felt down the upper extremity if it occurs in the cervical region or down the lower extremity if it occurs in the lumbar region.
Localized nerve pathologies that occur distal from the nerve roots are called peripheral neuropathies. A peripheral neuropathy may be caused by compression or tension forces applied to the nerve in one or more locations, including systemic disorders like multiple sclerosis or diabetes.
Massage, however, is more helpful in addressing localized mechanical compression and tension than systemic neuropathies, so that is our primary focus here.
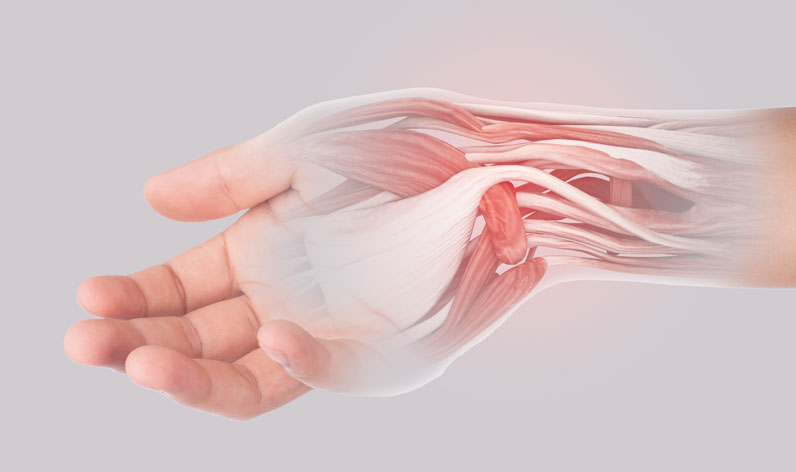
A mechanical peripheral neuropathy is caused by either excess compression or tension (pulling) on the nerve. Compression pathologies like carpal tunnel syndrome are generally more common than tension pathologies. Because the symptoms of neural tension injuries can be identical to compression pathologies, however, understanding both—especially when massage treatment plans for each may look different—is necessary.
Nerve compression injuries usually occur in regions where a nerve travels through a narrow pathway, such as a fibro-osseous tunnel. The nerve can get more easily compressed from within the tunnel because of the narrow space in the tunnel.
Nerves may also get compressed by fibrous bands in an adjacent muscle, cysts or tumors immediately adjacent to the nerve, or other obstructions along the nerve pathway.
Nerve Pathology Symptoms: Compression vs. Tension
Symptoms of nerve compression problems can be either motor or sensory. Motor symptoms include weakness and atrophy. If a motor nerve is being compressed, the muscles supplied by that nerve have an impaired signal and that’s what causes the weakness or atrophy.
Sensory symptoms usually produce paresthesia (pins and needles sensations), numbness, or sharp, shooting electrical-type pain. One of the unique factors of sensory nerve compression is that symptoms are most commonly felt distal to the site of compression, though this observation is a general guideline and not an absolute rule.
Massage therapists should consider reviewing the anatomy of the nervous system so they can recognize whether nerves in a particular region have a high concentration of motor fibers, sensory fibers, or a mixture of both.
In neural tension injuries, the nerve is overstretched. Nerves don’t have much natural elasticity, so they need to be somewhat slackened and capable of sliding back and forth in relation to adjacent tissues during limb movement.
When a nerve is not able to glide freely, neural tension problems may occur. Sometimes this happens because a nerve gets tethered or bound in one location while the other end is pulled, meaning it’s not able to glide freely throughout the extremity.
When a nerve is exposed to excessive tensile stress, the overall diameter of the nerve decreases as the nerve is stretched, which can produce the same symptoms as nerve compression.
A good analogy to understand this process is to think of the nerve as a piece of rubber surgical tubing. When stretched, the diameter of the tubing decreases and the contents of that tubing will get squeezed. This squeezing of the internal contents and excessive pulling of the nerve fibers are what produce the pathological sensations from neural tension.
Nerve Pathologies and the Injuries They Cause
When the nerve is impaired from either compression or tension, the axons and myelin sheath degenerate first. As damage continues, the connective tissue layers surrounding the nerve trunk and its individual fibers are eventually damaged, too.
The degeneration of the axon and myelin sheath is called wallerian degeneration. Because some of the connective tissue layers remain intact after the central components of the nerve are damaged, some supporting structure of the nerve is left intact. This remaining structure can provide a template for regeneration of axons if the damage is not severe.
The least severe nerve injury involves simply blocking axon conduction. The nerve continues to conduct some signals above and below the primary area of compression or injury, but conduction velocity slows. Common symptoms include mild sensory and motor deficits, which are usually alleviated when pressure is removed from the nerve.
A loss in continuity of the axon occurs in later stages of nerve pathology, though the surrounding endoneurium could still be intact. The outer layers of connective tissue are still intact as well.
Typical symptoms include sensory and motor dysfunction, as well as significant pain. If the connective tissue layers are intact, the nerve axon is likely to regenerate, although slowly. The rate of regeneration of nerve axons is estimated to be 1 millimeter per day or 1 inch per month, and slower in many cases.
More severe damage affects not only the axons, but also their connective tissue layers. Because these layers are damaged, recovery may not be possible. This type of damage occurs in severe crush injuries or situations where the nerve is severed.
Once-severed axons can regenerate, but because the connective tissue template is disrupted, the axons may not grow back in their original locations, which is one reason why people may experience altered sensations or function when regaining use after surgical repair.
Nerve Pathologies: Acute vs. Chronic
Neural compression and tension pathologies are either acute or chronic. Acute compression injuries occur with a direct blow to a nerve, such as the ulnar nerve near the olecranon process of the elbow (the region known as the funny bone). Acute tension injuries result from the sudden stretch of a nerve, such as in the brachial plexus with lateral whiplash during a side-impact automobile collision.
Chronic compression injuries develop with low levels of pressure that are left on the nerve for a long time. Nerve damage can occur even with very little pressure if it is applied over a significant period of time.
Low levels of pressure make some nerve compression injuries difficult to detect. Chronic tensile injuries can also develop even with low to moderate levels of tension on a nerve for long periods.
Chronic injuries are more likely to develop from repetitive occupational or recreational motions, postural distortion, or prolonged periods of mechanical stress on the nerve.
When possible, identify the mechanical demands of the occupation or recreational activity to determine if adverse compression or tension is placed on any particular nerve or nerve root.
For example, repetitive pronation of the forearm during occupational activities could cause the pronator teres muscle to compress the median nerve.
When possible, try to determine if sensations are increased with compression, stretching, or both. In some cases, compression and stretching occur simultaneously.
For example, if there is compression of the tibial nerve in the tarsal tunnel, neurological sensations may increase with ankle dorsiflexion as the nerve is stretched taut against adjacent structures (creating compression and tension). Knowledge of anatomy and the paths of peripheral nerves throughout the body is essential for this analysis.
I frequently hear massage therapists say the nervous system was not given a great deal of attention in their training programs. This is not unique to massage therapy training, as I have also heard similar statements from those in other allied health professions that deal with musculoskeletal disorders.
Understanding nerve compression and tension pathologies can greatly help you chart a course of treatment that will be most effective for your clients.